 The Centers for Medicare and Medicaid Services (CMS) may be weeks away from announcing staffing mandates for the nursing home industry as part of its multi-point reform plan announced in February 2022. Citing widespread failure of nursing homes to comply with federal guidelines, the agency has promised to propose minimum nursing home staffing requirements to ensure that residents receive the care they deserve. Brent Wieand, a Philadelphia nursing home lawyer, explains why nursing home understaffing is so prevalent in the industry, and why understaffing is a leading cause of neglect, abuse, and lack of quality care in the industry.
The Centers for Medicare and Medicaid Services (CMS) may be weeks away from announcing staffing mandates for the nursing home industry as part of its multi-point reform plan announced in February 2022. Citing widespread failure of nursing homes to comply with federal guidelines, the agency has promised to propose minimum nursing home staffing requirements to ensure that residents receive the care they deserve. Brent Wieand, a Philadelphia nursing home lawyer, explains why nursing home understaffing is so prevalent in the industry, and why understaffing is a leading cause of neglect, abuse, and lack of quality care in the industry.
Despite staffing recoveries in every other health care sector since the beginning of the pandemic, the nursing home industry is still wheeling from COVID staffing losses. These losses, which federal labor statistics estimate to be over 200,000 workers and over 15% of their total workforce, continue to plague nursing homes in Pennsylvania and nationwide. The American Health Care Association (ACHA) and the American Hospital Association (AHA) believe these staffing shortfalls will endure through 2027.
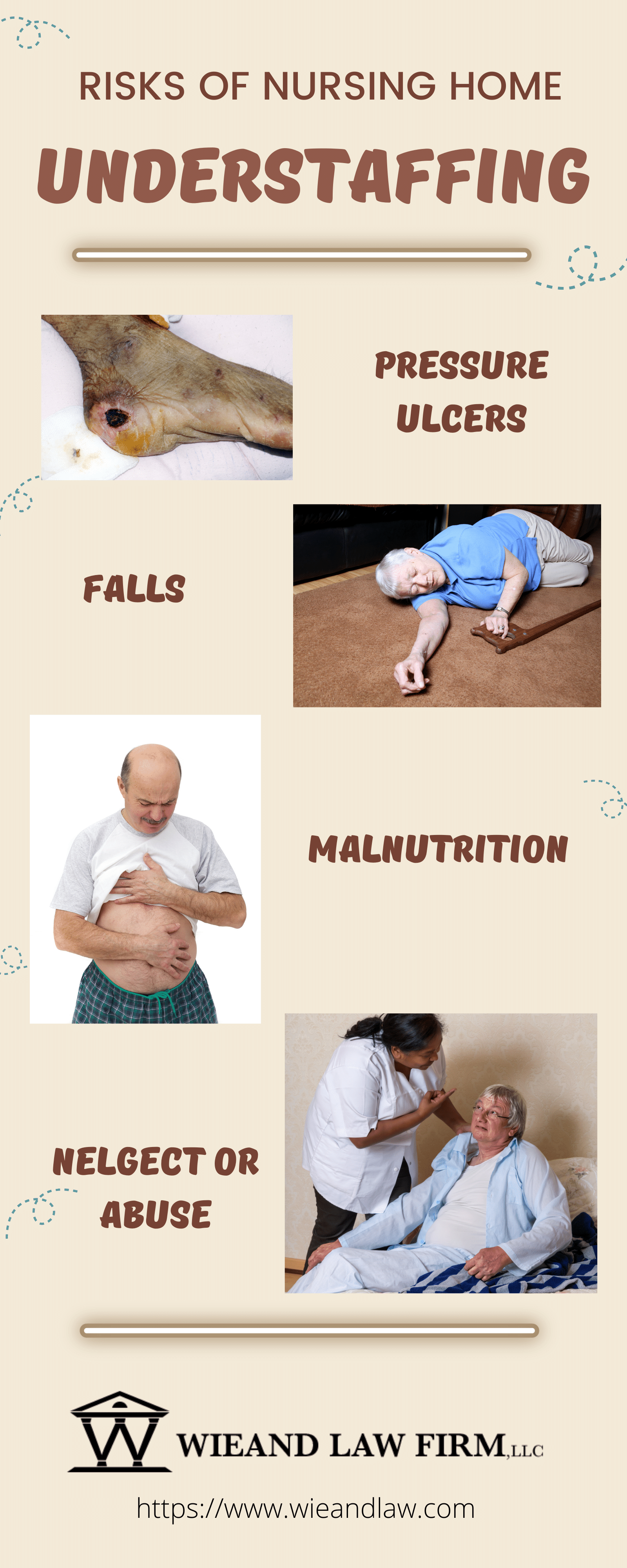
For Philadelphia nursing home lawyer, Brent Wieand, these staffing deficits have spurred a greater number of nursing home negligence lawsuits being filed his law firm. “Families are seeing the ramifications of nursing home understaffing as residents suffer from preventable pressure ulcers, falls, and infections. When working with nursing home administrators and owners fail to resolve quality issues, families are reaching out to the Wieand Law Firm to address their concerns through litigation.”
According to a Philadelphia nursing home lawyer at the Wieand Law Firm, residents at many Pennsylvania nursing homes continue to suffer from unsafe staffing conditions. Residents in understaffed facilities are at higher risk of suffering from pressure ulcers, malnutrition, dehydration, weight loss, and infections. Chronic understaffing is particularly prevalent in for-profit facilities, which comprise about 70% of U.S. nursing homes.
For-profit nursing homes and chains tend to operate with lower staffing and sustain higher quality deficiencies than their not-for-profit peers. Facilities who boast the highest profit margins have often been found to have the poorest quality outcomes. Many times, residents and their family members have needed to turn to nursing home negligence lawsuits to seek relieve from neglectful nursing home care.
 What Staffing Level is Adequate for Care?
What Staffing Level is Adequate for Care?Multiple studies have explored on nursing home staffing and its relationship to higher quality of care outcomes. Specifically, higher levels of registered nurses (RNs) and certified nursing assistants (CNAs) have been aligned with improved quality indicators, including pressure ulcers, pain management, and pressure ulcers.
A 2001 study by the Centers for Medicare and Medicaid Services (CMS) promoted a 4.1 minimum hours per patient day (PPD) in order to meet federal quality standards. This study, conducted over 20 years ago, may not fully capture the current day higher acuity needs at many of our nation’s nursing homes. Yet, the vast majority of nursing homes fail to meet this decades-old staffing recommendation.
When CMS launched its 5-star rating system for nursing homes, the agency developed a method to determine expected nurse staffing levels for each nursing home based on resident acuity. A 2016 examination of expected staffing levels accounting for resident acuity indicated that a typical nursing home should have 4.17 minimum PPD.
While no single standard has yet been identified within the industry, it’s well known that most nursing home staffing levels are subpar. Serious reform and established mandatory staffing levels are needed to ensure resident health and safety.
The Office of the Inspector General (OIG) found in 2014 that a third of Medicare nursing home residents experience adverse events that result in harm or death within the first 35 days of a skilled nursing stay. Of these adverse events, 60% were related to substandard treatment, inadequate monitoring, or treatment failures and delays.
Substandard nursing home staffing has been linked to several adverse events, including:
Overall, substandard nursing home staffing can have serious consequences for the health and well-being of residents.
Philadelphia nursing home lawyer, Brent Wieand, tirelessly advocates for the residents and families of nursing home residents who have suffered serious adverse events and wrongful death as a direct result of nursing home understaffing.
Mr. Wieand understands the imbalance in power between the nursing home industry and individual consumers. A staunch consumer advocate, Mr. Wieand seeks to end this imbalance by holding bad actors liable through nursing home negligence lawsuits. He believes that holding nursing home liable for their actions empower consumers to demand change and pave the way to nursing home reform.
 Proving Nursing Home Negligence in Pennsylvania
Proving Nursing Home Negligence in PennsylvaniaIn Pennsylvania, to prove nursing home negligence, a plaintiff must demonstrate the following elements:
Common claims in nursing home negligence lawsuits include that the nursing home:
To prove each of these elements, the plaintiff may need to present evidence such as medical records, witness statements, and expert testimony.
In addition, in Pennsylvania, nursing homes are required to comply with state and federal regulations related to resident care and safety. Violations of these regulations may be used as evidence of nursing home negligence.
It is important to note that nursing home negligence cases can be complex, and it may be necessary to consult with an experienced Philadelphia nursing home attorney to determine whether a valid claim exists and to navigate the legal process.
 Contact a Philadelphia Nursing Home Lawyer at the Wieand Law Firm Today
Contact a Philadelphia Nursing Home Lawyer at the Wieand Law Firm TodayIf your loved one has suffered serious injury or wrongful death at the hands of a neglectful nursing home provider, contact the Philadelphia nursing home lawyers at the Wieand Law Firm today. Call 215-666-7777 to speak directly with an attorney for a free case review and consultation.